Acute kidney injury occurs (AKI) in one out of four babies, children and young adults during an intensive care stay for any reason, and yet the condition is poorly understood. It is associated with various treatments or diagnostic procedures that hospitalized children undergo, and it is often the result of significant infection. About 15 percent of kids with AKI do not survive, compared to a 2 percent overall mortality rate for children requiring pediatric intensive care. Problematically, many children who experience AKI will need dialysis treatment and kids with AKI are at higher risk for chronic kidney disease later in life (one in three). Despite these alarming numbers, knowledge about this condition is limited and only recently has there been focus on the aspects of this disease process in children.
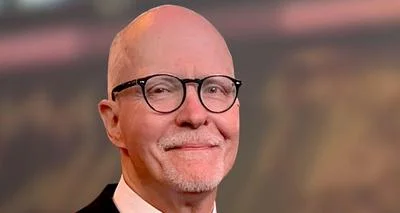
“At this stage, we are only at the cusp of understanding why AKI occurs, how to diagnose it early, track it in real time, prevent it, nor how to care for it. We don’t have standards to manage care for children and have been using adult recommendations. Children are unique and deserve their own precise directives,” said Rajit Basu, MD, MS, Division Head of Critical Care Medicine at Ann & Robert H. Lurie Children’s Hospital of Chicago, who chaired the first pediatric international conference on AKI that resulted in an expert consensus statement published in the journal JAMA Network Open. Dr. Basu is the senior author on this milestone publication, in which 46 global experts identify key issues in pediatric AKI and set a focused research agenda for the next five to 10 years. “It is a rallying cry for greater attention to this condition in children,” he said.
“In order to improve care and reduce the morbidity and mortality associated with AKI in kids, we need to understand more about the unique aspects of which populations of children are at highest risk, how to modernize our diagnostics, ways to incorporate and optimize therapeutics, how development and age (differences between babies and teenagers for instance) impact this wide-ranging condition, and the importance of nutrition, fluid accumulation and other factors that are unique to children,” said Dr. Basu, who also is a Professor of Pediatrics at Northwestern University Feinberg School of Medicine and holds the Posy and John Krehbiel Professorship in Critical Care Medicine. “This work helps the field organize and work together to establish guidelines and research for pediatric AKI and its various severity levels, and we need to develop evidence-based practice and research to drive quality care and better outcomes for these children. Within the last decade we have been accumulating more and more data that brought us to this exciting moment, but we’re just at the tip of the iceberg of our fight against AKI for children.”
Co-authors from Lurie Children’s also include Matthew Barhight, MD, and Theresa Mottes, APRN-NP, CPNP-AC, CDN.
Research at Ann & Robert H. Lurie Children’s Hospital of Chicago is conducted through Stanley Manne Children’s Research Institute. The Manne Research Institute is focused on improving child health, transforming pediatric medicine and ensuring healthier futures through the relentless pursuit of knowledge. Lurie Children’s is ranked as one of the nation’s top children’s hospitals by U.S. News & World Report. It is the pediatric training ground for Northwestern University Feinberg School of Medicine.
Original source can be found here.




 Alerts Sign-up
Alerts Sign-up